What You Should Know About Scoliosis
Back pain is one of the most common causes of disability. According to a 2018 survey, it affects 28% of men and 31% of women. One of the disorders that lead to back pain is scoliosis.
Source:
When viewed from the side, the spine has 3 normal curves located at the neck, chest, and lower back. Normal lordosis is the forward curve of the spine at the neck and lower back, while normal kyphosis is the backward curve at the chest and hip. These curves give the spine the ability to absorb shock and distribute stress during movement.
Patients with scoliosis have a spine that's curved to the side (either left or right), forming an 'S' shape. The curve is often present in the thoracic spine (chest) and measures at least 10 degrees on an X-ray. It affects 6-9 million people in the U.S.
What are the causes of scoliosis?
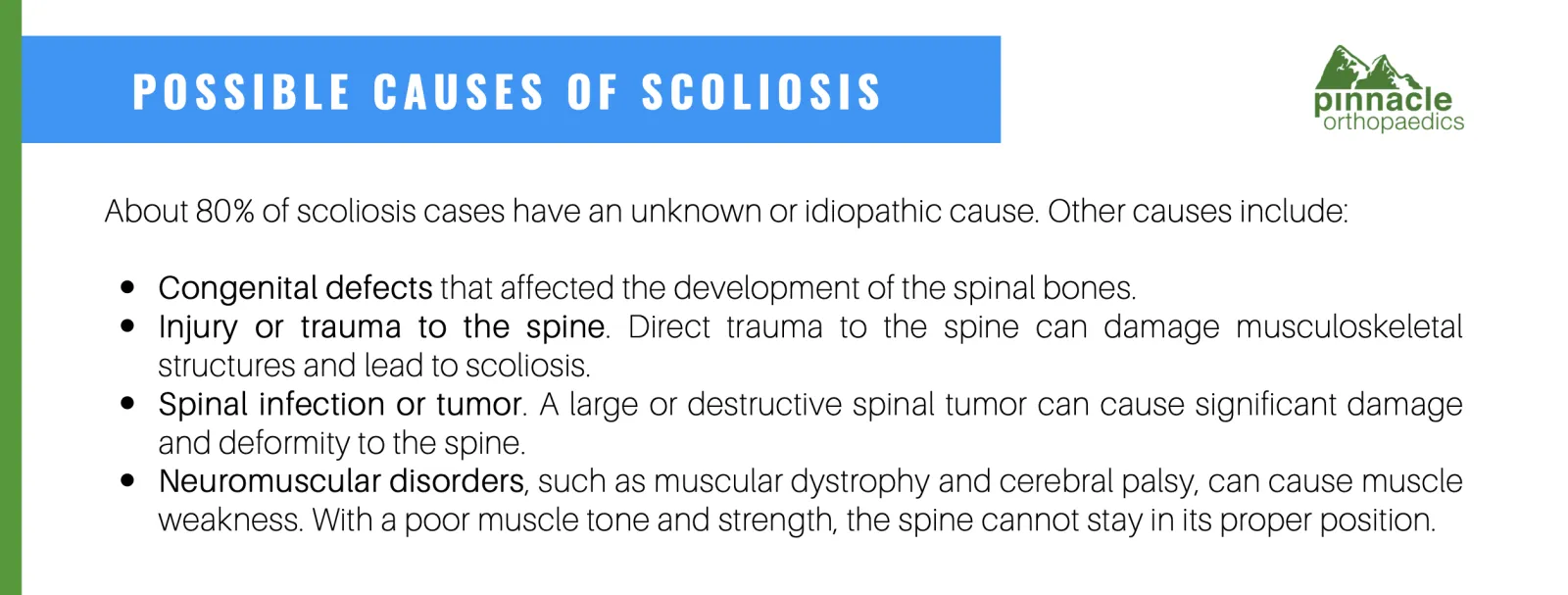
About 80% of scoliosis cases have an unknown or idiopathic cause. Other causes include:
Congenital defects that affected the development of the spinal bones.
Injury or trauma to the spine. Direct trauma to the spine can damage musculoskeletal structures and lead to scoliosis.
Spinal infection or tumor. A large or destructive spinal tumor can cause significant damage and deformity to the spine.
Neuromuscular disorders, such as muscular dystrophy and cerebral palsy, can cause muscle weakness. With a poor muscle tone and strength, the spine cannot stay in its proper position.
What are the signs and symptoms of scoliosis?
You might have scoliosis if you experience the following signs and symptoms:
Uneven shoulders
Uneven hips
Uneven waist
Uneven rib cages
Off-centered head
Back pain
What are the types of scoliosis?
Structural scoliosis
Structural scoliosis, the most common type of scoliosis, affects the structure of the spine. It involves some degree of spinal rotation and a sideways curve. The condition is permanent, and treatment is often necessary to correct the spinal deformity.
Structural scoliosis has 4 types, categorized according to the cause:
Idiopathic scoliosis
Idiopathic scoliosis has an unknown cause, although studies are being conducted to determine if genetics is a causative factor. It is the most common type of scoliosis that affects 8 out of 10 patients. Most patients with this type of scoliosis are diagnosed during their teenage years.
Idiopathic scoliosis is further categorized by age:
Infantile scoliosis develops from birth to age 3
Juvenile scoliosis develops from ages 4 to 9
Adolescent scoliosis develops from ages 10 to 18
Degenerative scoliosis
Also known as adult-onset scoliosis, it results from the degeneration of the joints and intervertebral discs in the spine. The degeneration is gradual, progressive, and may occur as a result of aging.
Neuromuscular scoliosis
Neuromuscular scoliosis, also called myopathic scoliosis, develops in patients with conditions that lead to muscle damage or muscle weakness. Examples of such conditions are muscular dystrophy and cerebral palsy.
Congenital scoliosis
Congenital scoliosis develops while the patient is still in the womb and is already present during infancy. It may be associated with spinal malformations.
This type of scoliosis is rare and only affects 1 in 10,000 patients. Because 20% of patients with congenital scoliosis have an associated spinal cord problem, it usually requires neurological and surgical intervention.
Non-structural scoliosis
Also termed functional scoliosis, this type of scoliosis is temporary and does not include spinal rotation. There is no damage to the musculoskeletal structure of the spine, and the scoliosis curve only appears when the patient is at certain positions.
Non-structural scoliosis is uncommon and may develop due to:
Muscle spasms. Spasms are involuntary muscle contractions. When a major back muscle spasms, it can pull the spine sideways towards its direction.
Leg asymmetry. Patients whose one leg is longer than the other may have a scoliosis curve when standing.
Inflammation. Having an inflamed organ on one side of the body, such as in the case of appendicitis and pneumonia, can lead to a scoliosis curve.
How is scoliosis diagnosed?
There are several ways to diagnose scoliosis, and your doctor may use a combination of these methods.
Clinical diagnosis
Your orthopedic doctor may ask questions about the symptoms you are experiencing, your family history, and medical history to clinically diagnose scoliosis. They may also perform a physical assessment and screening test.
Adam's Forward Bend Test is the standard test to screen for scoliosis. The doctor asks the patient to bend forward at the waist as he looks for signs of asymmetry. If the back is uneven, with one side higher than the other, the patient may have scoliosis.
A forward test cannot determine the type of scoliosis and the severity of the curve. Patients are advised to undergo imaging or radiographic tests to confirm the diagnosis and determine the best course of treatment.
Radiographic tests
Scoliosis can be confirmed through imaging tests, such as chest X-ray, CT scan, MRI, or spinal radiograph. Doctors use the Cobb Method to measure the severity of the curvature in degrees. The bigger the curvature, the more severe the scoliosis.
Mild scoliosis measures 10 to 20 degrees
Moderate scoliosis curve is between 25 to 40 degrees
Severe scoliosis is more than 50 degrees of curvature
What are the available scoliosis treatments?
The treatment for a confirmed case of scoliosis depends on the following factors:
Maturity of the spine. Is the spine already mature, or is it still growing?
Severity. What is the degree of curvature?
Curve location. What part of the spine is affected?
Curve progression. What is the possibility of the curve getting worse?
Impact on lifestyle. Do the signs and symptoms affect or limit the patient's lifestyle?
Your spine doctor takes into consideration the answers to these questions before recommending a combination of treatments, such as:
Observation
Lifestyle change and home remedies
Medications
Exercise
Brace
Surgery
Observation
Generally, patients with mild scoliosis do not require treatment. Children with mild scoliosis may be examined every 4 or 6 months for signs of progression. On the other hand, adults with scoliosis may be observed every five years for increasing curvature. During each consultation, the doctor may recommend an X-ray of the spine to see if the curve is getting worse.
Lifestyle and home remedies
Weight management. Patients with degenerative scoliosis are advised to maintain a healthy weight. Losing weight can help decrease the pressure in the spinal joints, reduce pain, and delay curve progression.
Nutrition. Eating foods with anti-inflammatory properties, such as ginger and turmeric, can help relieve inflammation in patients with degenerative scoliosis.
Hydration. Drinking at least 8 glasses of water a day can keep your spinal joints lubricated.
Warm or cold compress. Back pain is a common complaint of patients with scoliosis. The abnormal curvature of the spine can put pressure on adjacent nerves. It can also shift the position of your ribcage and strain the muscles in the back, leading to localized back pain. A warm compress can help relax back muscles and increase blood flow to the area, while a cold compress can reduce localized inflammation and relieve pain.
Posture. Patients with scoliosis may notice that prolonged sitting can lead to pain, stiffness, and tightness of the back muscles. Maintaining proper posture and using proper body mechanics can help minimize the stress to these muscles and decrease back pain episodes.
Medications for scoliosis
Scoliosis medications are usually given to provide symptomatic relief, but they cannot cure the deformity itself.
Patients with degenerative scoliosis may be given pain medications to help them manage pain during physical therapy. Your doctor may give pain killers orally or through epidural steroid and facet block injections.
Examples of oral pain relievers are nonsteroidal anti-inflammatory drugs or NSAIDs (ibuprofen and aspirin) and acetaminophen (paracetamol and Tylenol).
Epidural steroid injection involves the injecting of steroid medication into the epidural space. On the other hand, facet block injections involve injecting a local anesthetic agent into a facet joint. Both of these minimally invasive procedures can block pain in the target area.
Back braces for scoliosis
Braces are effective in patients whose spine hasn't reached full skeletal maturity. In a 2015 study published in the Scoliosis Journal, it has been concluded that brace treatment can effectively stabilize 76% of adolescent idiopathic scoliosis.
Spine doctors may advise children with 25 to 40 degrees of spinal curvature to wear a brace to prevent progression. Bracing treatment is also considered if the curve has progressed by at least 5 degrees during the 4-6 month observation stage.
Braces should be properly fitted and worn at least 16 to 23 hours daily until the bones are fully matured. The success rate of bracing depends on the patient's compliance and the number of hours the brace is worn.
Wearing the brace for 8 hours a day has 60% success rate
Wearing the brace for 16 hours a day has 62% success rate
Wearing the brace for 23 hours a day has 93% success rate
Exercises for scoliosis
Back exercises can help improve your posture and keep the back and abdominal muscles flexible and strong enough to support the spine. Some of these scoliosis exercises include pelvic tilt, cat and cow stretch, arm raise, and leg raise.
Patients can also get the help of a physiotherapist for scoliosis specific-exercises. The goals of physiotherapy are to:
prepare patients for wearing a brace
train patients to correct their posture on their own
improve posture by strengthening muscles
reshape the chest
correct the scoliosis curve
keep the normal curves of the spine
Surgery for scoliosis
Surgery is the last resort to treat scoliosis. For children with scoliosis, experts recommend surgery when the curve is more than 40 degrees and shows signs of progression. For adults to qualify for surgery, the curve must be more than 50 degrees and is associated with nerve damage and bladder and bowel problems.
Patients with degenerative scoliosis may need to have decompression surgery in addition to spinal fusion surgery to relieve the pressure from the nerves.
